CHARLES LINDQUIST, DC, MS / PATIENT / MAY 20, 2024
Introduction:
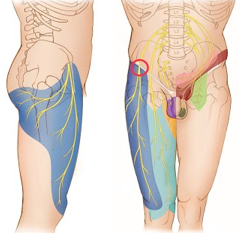
Meralgia Paresthetica (MP) is a neurologic condition characterized by the entrapment or compression of the lateral femoral cutaneous nerve (LFCN) as it traverses beneath the inguinal ligament. In recent years, its prevalence has surged, paralleling the rise in obesity rates. This review aims to provide a comprehensive overview of MP for healthcare professionals, focusing on its etiology, clinical presentation, diagnostic approach, and management strategies.
Etiology and Risk Factors:
MP often arises due to external compression of the LFCN, leading to sensory disturbances in the lateral thigh region. Several factors contribute to nerve compression, including obesity, seatbelt injuries, mechanical stress from twisting under load, and various intra-abdominal compressive conditions such as tight clothing, hernias, muscular spasm, and pregnancy. Notably, there exists a significant association between MP and metabolic conditions like obesity, diabetes, and age, underscoring the multifactorial nature of its etiology.
Clinical Presentation and Differential Diagnosis:
Patients with MP typically present with sensory symptoms localized to the lateral thigh, including tingling, numbness, or burning sensations. While pain may predominate, weakness in the affected leg can also be reported. However, distinguishing MP from other common conditions, such as sciatica, sprains, plexopathy, or radiculopathy, is paramount. A thorough clinical evaluation, coupled with a detailed patient history and targeted physical examination, is essential for accurate diagnosis and appropriate management.
Diagnostic Approach:
Diagnostic challenges often accompany MP due to its overlapping symptomatology with other conditions. Electrodiagnostic studies, though infrequently utilized, can aid in confirming the diagnosis by assessing nerve conduction and detecting abnormalities in nerve function. Physical examination techniques, including abdominal assessment and digital compression of the LFCN at the inguinal ligament, can help reproduce symptoms and guide diagnostic decisions. Imaging modalities such as ultrasound or MRI may also be employed to visualize nerve compression or rule out other pathologies.
Management Strategies:
The management of MP encompasses a multimodal approach tailored to individual patient needs. Conservative measures play a pivotal role and may include weight management, physical therapy focusing on muscle strengthening and flexibility, avoidance of constrictive clothing, and corticosteroid injections to alleviate inflammation. Patients refractory to conservative measures may benefit from surgical interventions such as nerve release or hernia repair to decompress the LFCN and alleviate symptoms.
Conclusion:
In conclusion, MP poses a diagnostic and therapeutic challenge for healthcare professionals, necessitating a multidisciplinary approach for optimal patient care. By fostering collaboration between physicians and therapists and employing evidence-based practices, clinicians can effectively diagnose, manage, and mitigate the impact of MP on patient quality of life. Continued research efforts aimed at elucidating its pathophysiology and refining treatment strategies are essential for advancing our understanding and improving outcomes in patients with MP.
Share this post: on Twitter on Facebook on Google+
















